Your Child's Nasogastric Tube: Syringe Feeding
Your child is going home with a nasogastric (NG) feeding tube in place. This is a soft thin tube put into your child’s nose and down into the stomach. It sends liquid food directly to the stomach. You’ll need to feed your child through this tube. You were shown how to do this before your child came home from the hospital. This sheet will help you remember those steps at home. If you need more help, talk with the hospital. They can tell you how to arrange a home health nurse to help you.
Keep in mind that there are many types of NG tubes and syringes. Your child’s NG tube and supplies may look or work differently from what are described and shown here. Follow your child's care team's directions for your child's NG tube.
Take care to keep the tube from becoming a strangulation risk to your child. Follow your healthcare team's advice on how to secure the tube safely.
Contact information to keep handy
Ask for phone numbers to call if you need help. Also make sure you have the phone number for your child’s medical supply company. You’ll need to order more supplies for your child in the future. Write all of these phone numbers below.
Healthcare provider phone number: ____________________________________
Home health nurse phone number: _____________________________________
Medical supply company phone number: __________________________________
Types of feeding
There are 2 types of feeding with an NG tube. Your child may have 1 or both types of feeding. They are:
-
Continuous feeding. Liquid food is dripped slowly through the tube for part or all of a day. This type of feeding is only done using a pump. The amount of food to be given and time frame are often set on the pump for you. Don't change pump settings unless you’re instructed to do so.
-
Bolus feeding. This is a meal-sized amount of liquid food. It's given through the tube several times a day. Bolus feeding is given using a syringe or a pump. Your child’s healthcare provider or home health nurse will tell you how much liquid food to use for each feeding. You’ll also be told how often to feed your child.
For bolus feeding, fill in the numbers below:
Feed your child on this schedule: ____________________________________________
Give this much at each feeding: ______________________________________________
Checking tube placement before feeding
Every time you feed your child, you’ll need to be sure the NG tube is in the correct place. The end of the tube must be in your child’s stomach. It should not be in the lungs or throat. To check if the tube is in place, draw some liquid from the stomach and test it. Do this check before each feeding.
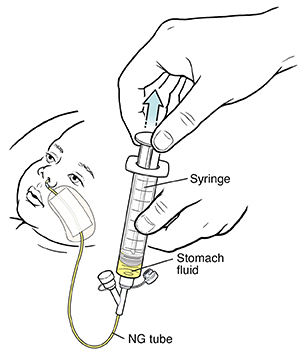
The supplies you’ll need are:
-
Syringe
-
pH testing strips
Follow these steps:
-
Wash your hands with soap and water.
-
Attach the syringe to the end of the NG tube. Make sure the other port of the tube is closed off.
-
Pull back on the plunger of the syringe. Do this until you see liquid from the stomach in the syringe.
-
Look at the color of the fluid. It should look clear or light yellow.
-
Check the pH of the liquid from the stomach using pH paper. Stomach (gastric) pH should be 1 to 5 if your child isn't taking a proton pump inhibitor or H2 receptor antagonist. There are things that can increase pH. Follow your provider's specific instructions.
-
If you aren't sure the tube is in the stomach, don’t go ahead with the feeding. Re-insert or gently move the NG tube as you were instructed at the hospital. Repeat the above steps to check for correct placement.
-
Remove the syringe from the feeding tube.
-
Tape the tube securely in place along your child’s nose or cheek. Do this as you were shown in the hospital.
-
Wash the syringe out with soap and water and allow to dry.
-
Go ahead with feeding as instructed.
Feeding your child
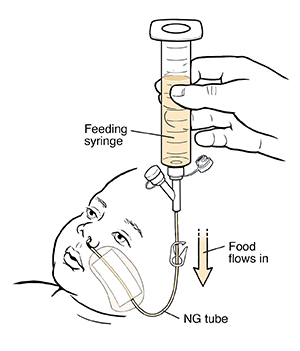
After checking the tube placement, feed your child the amounts on the schedule as noted above.
The supplies you’ll need are:
-
Liquid food
-
Feeding syringe
Follow these steps:
-
Wash your hands with soap and clean, running water.
-
Check the label and expiration date of the liquid food. Don’t use any can or bag of food if the expiration date has passed. Instead, get a new can or bag of food.
-
Open the feeding port cap at the end of the NG tube.
-
Pull the plunger out of the feeding syringe.
-
Connect the feeding syringe to the feeding port of the NG tube.
-
Gently bend or pinch the tube with one hand. Keep bending or pinching the tube. At the same time, slowly pour the food into the feeding syringe with your other hand. This keeps the food from flowing through the tube until you are done measuring it.
-
Fill the feeding syringe only to the amount prescribed by your child’s healthcare provider.
-
Release the hand that is bending or pinching the tube.
-
Hold the feeding syringe straight up. This allows the food to run through the tube by gravity. Change the angle of the feeding syringe to control the flow rate of the food.
-
If the food flows too slowly or doesn’t flow at all, place the plunger in the syringe. Gently push the plunger a bit. This can help remove anything that is blocking or clogging the tube. Don't push the plunger all the way into the syringe or with force.
-
Refill the feeding syringe with food, if needed. Repeat steps until your child has had the prescribed amount of food.
-
After the feeding, flush the tube with water as you were shown in the hospital.
-
Disconnect the feeding syringe.
-
Close the feeding port cap of the tube.
Additional instructions: _____________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
When to call the healthcare provider
Call the healthcare provider right away if any of these occur:
-
You can't place the tube.
-
The skin around the tube site has redness, swelling, leaking fluid, or sores.
-
You see blood around the tube, in your child’s stool, or in the stomach contents.
-
Your child coughs, chokes, or vomits while feeding.
-
Your child’s belly looks bloated or feels hard when gently pressed.
-
Your child has diarrhea or constipation.
-
Your child has a fever (see "Fever and children" below)
Call 911
Call 911 or get medical care right away if:
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older